International Perspectives:I thought it would be interesting to periodically have some of my international colleagues and friends contribute to Residency Insight. The purpose is twofold; first, it gives you a break from having to "listen" to me each month in these issues. Secondly and more importantly, it gives you the international perspective that you need to practice effectively. I've said before that it's a big world out there. Yet, there is a relatively small and cohesive group of diabetic foot specialists that make up the international foot care community. They are all unique, dedicated, and have valuable experiences to share with their colleagues. This issue has been contributed by a leading diabetic foot specialist from Milan, Italy. Dr. Giacomo Clerici is a trained diabetologist who also performs podiatric surgery at the Casa di Cura Multimedica (Milano), where he is the Chief of the Diabetic Foot Unit. A well published author and researcher on diabetic foot ischemia and infections, I am pleased to introduce you to my good friend who will discuss his perspective on the ischemic diabetic foot.  —Robert Frykberg, DPM, MPH, PRESENT Editor, Diabetic Limb Salvage
Ischemic Diabetic Foot: change in the pattern
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
More problems
Notwithstanding the increase of surgical revascularizations, the major amputation rates still remained high, albeit improved, during the middle of the 1990s. The explanation was owing to the fact that many patients were still excluded from surgical revascularisation due to clinical conditions (elderly patients, with many comorbidities) or for a poor run off (absence of a distal arterial target vessel that could “accept” the by-pass).
Even now, most of the scientific articles available in the literature that report the outcomes of open revascularization concern selected patient statistics, not those consecutively enrolled. Therefore, in these case series, it is unknown how many patients have been excluded, the reason for the exclusion and their eventual outcomes. Even in our own experience, the patients excluded from surgical revascularization for the above reasons were many indeed!
The rationale for HBO use in the ‘90s
With the aim to further decrease the number of amputated patients and to fill that gap created by the exclusion of many ischemic patients from surgical revascularization in the middle of the ’90s, there was an explosion in the utilization of hyperbaric therapy (HBO). (Tragically, a real explosion happened a few years later in Milan, with the explosion of an hyperbaric chamber in a hospital that caused some deaths). This approach was enhanced also from the randomised paper of Ezio Faglia published on Diabetes Care in 1996, where a beneficial effect of HBO as adjuvant therapy was demonstrated.
Notwithstanding the promising results, it remained evident that the only therapy really effective in the reduction of the number of amputated patients was the direct revascularization down to the foot!
The Search for the ideal revascularization
Elderly patients with many comorbidities, mainly cardiac, were still in need of a revascularization that was ideally not very invasive, had little stress for the patient, did not require general anesthesia, and resulted in very few complications both intra and postoperative.
Angioplasty (PTA) was very close to this definition: it was and still is a mildly invasive procedure, only requires a local anesthesia and does not cause serious dermal lesions. In addition, the peri- and post-operative mortality is very low and the complications, even if present, are rare.
Based on the early experiences and publications of the Italian pioneers Ezio Faglia and Lanfroi Graziani (after those of Isner) there was a surge in PTA procedures being performed in neuroischemic diabetic patients in Italy. In the late 90s and the beginning of 2000, the experiences on consecutive cases (i.e. not selected) were reported, culminating with studies that had enrolled up to 1000 consecutive patients affected by an ischemic diabetic foot. The results were quite impressive compared to what existed only a few years before: the amputation rate in some Italian centres for diabetic foot care was reduced to 5% and remains at this level today.
Despite our results, international literature continued to recommend revascularization with PTA only for short arterial and focal stenoses or occlusion: certainly not those long, multilevel, calcific lesions that are so common in diabetics.
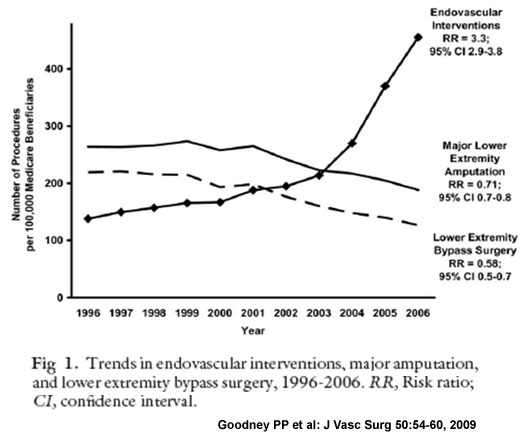
To illustrate what happened in these extraordinary years, the Ontario Study at first and, more recently, the scientific articles of Goodney, well describe the change in the pattern of revascularization in the last decade. (see Figure 1 below)
|
 |
And what of open surgery?
It is important to emphasize that PTA represents a method of revascularization that is not an alternative to by-pass. Today, in many diabetic foot centres, the capability to revascularize a patient affected by critical limb ischemia is equal to 95% (at the beginning of 1990s it was around 20%) and this is due to the utilization of both endovascular and surgical methods. It is unimaginable today to think that critical and chronic ischemia can be addressed with only one of the two techniques.
Our personal choice, based upon the minimally invasive nature and minor attendant complications, is PTA as a first revascularization strategy. Nonetheless, when this technique is not possible or when not effective, then by-pass, if possible, is utilized to solve the problem.
 |
In our center, we utilize PTA in 70% of patients affected by critical limb ischemia and the BPG (bypass graft) in 25%. In 5% of cases, we are not able to offer any type of revascularization. In Bologna, for example, Prof. Stella and Prof. Gargiulo (both vascular surgeons) have a PTA/BPG rate equal to 50%. Above all, the main concept is still the same: the utilization of both the techniques increases the numbers of revascularized patients and the rate of limb salvage.
Does revascularization mean limb salvage?
It is important to point out that revascularization does not always result in limb salvage. We have assisted, and we still assist today, to brilliant revascularizations followed by a major amputation. Why? Because we often forget that revascularization represents a part of the therapeutic process of the patient and not the whole process.
It is of vital importance emphasize that foot care must follow every phase of the treatment. Proper offloading, the correct treatment of infections, debridement, and the correct medications are integral parts of the process to reach final recovery.
 |
A typical example is the patient with a foot abscess andlimb ischemia: revascularization of this patient instead of an immediate surgical drainage (also in presence of ischemia), represents a serious delay in appropriate treatment, further tissue loss, and could lead to amputation.
If the patient is not urgently taken to the operating theatre, drained and subsequently revascularized (by and not later than 2 days from the urgent drainage) it will be difficult to save the soft tissues so precious for the final intervention. To lose time in the presence of a moderate or severe infection means, sometimes, a life threatening condition.
In this regard, proper management of the foot lesion represents that therapeutic part of overall care without which, even with the best of blood flow, will not achieve salvage of the limb.
### |
Please be sure to share your thoughts and comments in our eTalk forum. See you next time.
Get a steady stream of all the NEW PRESENT Podiatry eLearning by becoming our Facebook Fan. Effective eLearning and a Colleague Network await you. |
 |
PRESENT eZines are made possible through the support of our sponsors: |
|
||||
Major Sponsors |
||||